I. Personalized, Collaborative and Multidisciplinary Management
FAHZU is a designated hospital for COVID-19 patients, especially severe and critically ill individuals whose condition changes rapidly, often with multiple organs infected and requiring the support from the multidisciplinary team (MDT). Since the outbreak, FAHZU established an expert team composed of doctors from the Departments of Infectious Diseases, Respiratory Medicine, ICU, Laboratory Medicine, Radiology, Ultrasound, Pharmacy, Traditional Chinese Medicine, Psychology, Respiratory Therapy, Rehabilitation, Nutrition, Nursing, etc. A comprehensive multidisciplinary diagnosis and treatment mechanism has been established in which doctors both inside and outside the isolation wards can discuss patients’ conditions every day via video conference. This allows for them to determine scientific, integrated and customized treatment strategies for every severe and critically ill patient.
Sound decision-making is the key to MDT discussion. During the discussion, experts from different departments focus on issues from their specialized fields as well as critical issues to diagnoses and treatment. The final treatment solution is determined by experienced experts through various discussions of different opinions and advice.
Systematic analysis is at the core of MDT discussion. Elderly patients with underlying health conditions are prone to becoming critically ill. While closely monitoring the progression of COVID-19, the patient’s basic status, complications and daily examination results should be analyzed comprehensively to see how the disease will progress. It is necessary to intervene in advance to stop the disease from deteriorating and to take proactive measures such as antivirals, oxygen therapy, and nutritional support.
The goal of MDT discussion is to achieve personalized treatment. The treatment plan should be adjusted to each person when considering the differences among individuals, courses of disease, and patient types.
Our experience is that MDT collaboration can greatly improve the effectiveness of the diagnosis and treatment of COVID-19.
II. Etiology and Inflammation Indicators
1、Detection of SARS-CoV-2 Nucleic Acid
1.1 Specimen Collection
Appropriate specimens, collection methodds and collection timing are important to improve detection sensitivity. Specimen types include: upper airway specimens (pharyngeal swabs, nasal swabs, nasopharyngeal secretions), lower airway specimens (sputum, airway secretions, bronchoalveolar lavage fluid), blood, feces, urine and conjunctival secretions. Sputum and other lower respiratory tract specimens have a high positive rate of nucleic acids and should be collected preferentially. SARS-CoV-2 preferentially proliferates in type II alveolar cells (AT2) and peak of viral shedding appears 3 to 5 days after the onset of disease. Therefore, if the nucleic acid test is negative at the beginning, samples should continue to be collected and tested on subsequent days.
1.2 Nucleic Acid Detection
Nucleic acid testing is the preferred method for diagnosing SARS-CoV-2 infection. The testing process according to the kit instructions is as follows: Specimens are pre-processed, and the virus is lysed to extract nucleic acids. The three specific genes of SARS-CoV-2, namely the Open Reading Frame 1a/b (ORF1a/b), nucleocapsid protein (N), and envelope protein (E) genes, are then amplified by real-time quantitative PCR technology. The amplified genes are detected by fluorescence intensity. Criteria of positive nucleic acid results are: ORF1a/b gene is positive, and/or N gene/E gene are positive.
The combined detection of nucleic acids from multiple types of specimens can improve the diagnostic accuracy. Among patients with confirmed positive nucleic acid in respiratory tract, about 30% – 40% of these patients have detected viral nucleic acid in the blood and about 50% – 60% of patients have detected viral nucleic acid in feces. However, the positive rate of nucleic acid testing in urine samples is quite low. Combined testing with specimens from respiratory tract, feces, blood and other types of specimens is helpful for improving the diagnostic sensitivity of suspected cases, monitoring treatment efficacy and the management of post-discharge isolation measures.
2、Virus Isolation and Culture
Virus culture must be performed in a laboratory with qualified Biosafety Level 3 (BSL-3). The process is briefly described as follows: Fresh samples of the patient’s sputum, feces, etc. are obtained and inoculated on Vero-E6 cells for virus culture. The cytopathic effect (CPE) is observed after 96 hours. Detection of viral nucleic acid in the culture medium indicates a successful culture. Virus titer measurement: After diluting the virus stock concentration by a factor of 10 in series, the TCID50 is determined by the micro-cytopathic method. Otherwise, viral viability is determined by plaque forming unit (PFU).
3、Detection of Serum Antibody
Specific antibodies are produced after SARS-CoV-2 infection. Serum antibody determination methods include colloidal gold immunochromatography, ELISA, chemiluminescence immunoassay, etc. Positive serum-specific IgM, or specific IgG antibody titer in the recovery phase ˫4 times higher than that in the acute phase, can be used as diagnostic criteria for suspected patients with negative nucleic acid detection. During follow-up monitoring, IgM is detectable 10 days after symptom onset and IgG is detectable 12 days after symptom onset. The viral load gradually decreases with the increase of serum antibody levels.
4、Detecting Indicators of Inflammatory Response
It is recommended to conduct tests of C-reactive protein, procalcitonin, ferritin, D-dimer, total and subpopulations of lymphocytes, IL-4, IL-6, IL-10, TNF-ơ, INF-ƣ and other indicators of inflammation and immune status, which can help evaluate clinical progress, alert severe and critical tendencies, and provide a basis for the formulation of treatment strategies.
Most patients with COVID-19 have a normal level of procalcitonin with significantly increased levels of C-reactive protein. A rapid and significantly elevated C-reactive protein level indicates a possibility of secondary infection. D-dimer levels are significantly elevated in severe cases, which is a potential risk factor for poor prognosis. Patients with a low total number of lymphocytes at the beginning of the disease generally have a poor prognosis. Severe patients have a progressively decreased number of peripheral blood lymphocytes. The expression levels of IL-6 and IL-10 in severe patients are increased greatly. Monitoring the levels of IL-6 and IL-10 is helpful to assess the risk of progression to a severe condition.
5、Detection of Secondary Bacterial or Fungal Infections
Severe and critically ill patients are vulnerable to secondary bacterial or fungal infections. Qualified specimens should be collected from the infection site for bacterial or fungal culture. If secondary lung infection is suspected, sputum coughed from deep in the lungs, tracheal aspirates, bronchoalveolar lavage fluid, and brush specimens should be collected for culture. Timely blood culture should be performed in patients with high fever. Blood cultures drawn from peripheral venous or catheters should be performed in patients with suspected sepsis who had an indwelling catheter. It is recommended that they take blood G test and GM test at least twice a week in addition to fungal culture.
6、Laboratory Safety
Biosafety protective measures should be determined based on different risk levels of experimental process. Personal protection should be taken in accordance with BSL-3 laboratory protection requirements for respiratory tract specimen collection, nucleic acid detection and virus culture operations. Personal protection in accordance with BSL-2 laboratory protection requirement should be carried out for biochemical, immunological tests and other routine laboratory tests. Specimens should be transported in special transport tanks and boxes that meet biosafety requirements. All laboratory waste should be strictly autoclaved.
III. Imaging Findings of COVID-19 Patients
Thoracic imaging is of great value in the diagnosis of COVID-19, monitoring of therapeutic efficacy, and patient discharge assessment. A high-resolution CT is highly preferable. Portable chest X-rays are helpful for critically ill patients who are immobile. CT for baseline evaluation of patients with COVID-19 is usually performed on the day of admission, or if ideal therapeutic efficacy is not reached, it can be re-performed after 2 to 3 days. If symptoms are stable or improved after treatment, the chest CT scan can be reviewed after 5 to 7 days. Daily routine portable chest X-rays are recommended for critically ill patients.
COVID-19 at the early stage often presents with multifocal patchy shadows or ground glass opacities located in the lung periphery, subpleural area, and both lower lobes on chest CT scans. The long axis of the lesion is mostly parallel to the pleura. Interlobular septal thickening and intralobular interstitial thickening, displaying as subpleural reticulation namely a “crazy paving” pattern, is observed in some ground glass opacities. A small number of cases may show solitary, local lesions, or nodular/ patchy lesion distributed consistent with bronchus with peripheral ground glass opacities changes. Disease progression mostly occurs in the course of 7-10 days, with enlarged and increased density of the lesions compared with previous images, and consolidated lesions with air bronchogram sign. Critical cases may show further expanded consolidation, with the whole lung density showing increased opacity, sometimes known as a “white lung”. After the condition is relieved, the ground glass opacities can be completely absorbed, and some consolidation lesions will leave fibrotic stripes or subpleural reticulation. Patients with multiple lobular involvement, especially those with expanded lesions should be observed for disease exacerbation. Those with typical CT pulmo-nary manifestations should be isolated and undergo continuous nucleic acid tests even if the nucleic acid test of SAR-CoV-2 is negative.
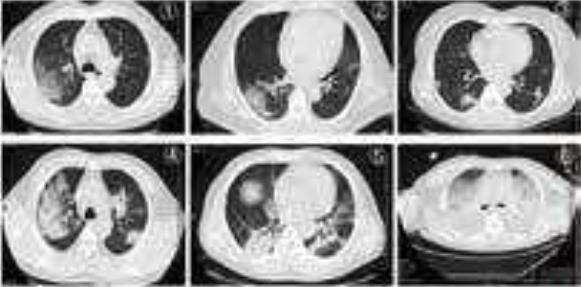
Figure 6: diffuse consolidation, “white lung”.21Handbook of COVID-19 Prevention and Treatment
Flexible bronchoscopy is versatile, easy to use, and well tolerated in mechanically ventilated COVID-19 patients. Its applications include:
(1) Collection of respiratory specimens from the lower respiratory tract (i.e. sputum, endotracheal aspirate, bronchoalveolar lavage) for SARS-CoV-2 or other pathogens guides the selection of appropriate antimicrobials, which may lead to clinical benefits. Our experi–ence indicates that lower respiratory specimens are more likely to be positive for SAR-CoV-2than upper respiratory specimens.
(2) Can be used for localization of the site of bleeding, cessation of hemoptysis, sputum or blood clots removal; if the site of bleeding is identified by bronchoscopy, local injection of cold saline, epinephrine, vasopressin, or fibrin as well as laser treatment can be performed via the bronchoscope.
(3) Assist in the establishment of artificial airways; guide tracheal intubation or percutane–ous tracheotomy.
(4) Drugs such as infusion of α-interferon and N-acetylcysteine can be administrated via the bronchoscope.Bronchoscopic views of extensive bronchial mucosal hyperemia, swelling, mucus-like secretions in the lumen and jelly-like sputum blocking the airway in critically ill patients. (Figure 7).
Bronchoscopic views of extensive bronchial mucosal hyperemia, swelling, mucus-like secretions in the lumen and jelly-like sputum blocking the airway in critically ill patients. (Figure 7).

Figure 7: Bronchoscopic manifestations of COVID-19: bronchial mucosa swelling and congestion; large amounts of mucus secretions in the lumen
V. Diagnosis and Clinical Classification of COVID-19
The diagnostic criteria follow Protocols for the Diagnosis and Treatment of COVID-2019. A confirmed case is based on epidemiological history (including cluster transmission), clinical manifestations (fever and respiratory symptoms), lung imaging, and results of SARS-CoV-2 nucleic acid detection and serum-specific antibodies.
Clinical Classifications:
1、Mild Cases
The clinical symptoms are mild and no pneumonia manifestations can be found in imaging
2、Moderate Cases
Patients have symptoms such as fever and respiratory tract symptoms, etc. and pneumonia manifestations can be seen in imaging
3、Severe Cases
Adults who meet any of the following criteria: respiratory rate ≥ 30 breaths/min; oxygen saturation ≤ 93% at a rest state; arterial partial pressure of oxygen (PaO2)/oxy-gen concentration (FiO2) ≤ 300 mmHg. Patients with > 50% lesions progression within 24 to 48 hours in lung imaging should be treated as severe cases.
4、Critical Cases
Meeting any of the following criteria: occurrence of respiratory failure requiring mechanical ventilation; presence of shock; other organ failure that requires monitoring and treatment in the ICU.
Critical cases are further divided into early, middle and late stages according to the oxygenation index and compliance of respiratory system.
●Early stage: 100 mmHg <oxygenation index ≤150 mmHg; compliance of respiratory system ≥30 mL / cmH2O; without organ failure other than the lungs. The patient has a great chance of recovery through active antiviral, anti-cytokine storm, and supportive treatment.
●Middle stage: 60 mmHg < oxygenation index ≤100 mmHg; 30 mL/cmH2O > compliance of respiratory system ≥15 mL/cmH2O; may be complicated by other mild or moderate dysfunction of other organs.
●Late stage: oxygenation index ≤ 60 mmHg; compliance of respiratory system <15 mL/cmH2O; diffuse consolidation of both lungs that requires the use of ECMO; or failure of other vital organs. The mortality risk is significantly increased.
VI. Antiviral Treatment for Timely Elimination of Pathogens
An early antiviral treatment can reduce the incidence of severe and critical cases. Although there is no clinical evidence for effective antiviral drugs, currently the antiviral strategies based on the characteristics of SAR-CoV-2 are adopted according to Protocols for Diagnosis and Treatment of COVID-19: Prevention, Control, Diagnosis and Management.
1、Antiviral Treatment
At FAHZU, lopinavir/ritonavir (2 capsules, po q12h) combined with arbidol (200 mg po q12h) were applied as the basic regimen. From the treatment experience of 49 patients in our hospital, the average time to achieve negative viral nucleic acid test for the first time was 12 days (95% CI: 8-15 days). The duration of negative nucleic acid test result (negative for more than 2 times consecutively with interval ≥ 24h) was 13.5 days (95% CI: 9.5 – 17.5 days).
If the basic regimen is not effective, chloroquine phosphate can be used on adults between 18-65 years old (weight ≥ 50 kg: 500 mg bid; weight ≤50 kg: 500 mg bid for first two days, 500 mg qd for following five days).
Interferon nebulization is recommended in Protocols for Diagnosis and Treatment of COVID-19. We recommend that it should be performed in negative-pressure wards rather than general wards due to the possibility of aerosol transmission.
Darunavir/cobicistat has some degree of antiviral activity in viral suppression test in vitro, based on the treatment experience of AIDS patients, and the adverse events are relatively mild. For patients who are intolerant to lopinavir/ritonavir, darunavir/ cobici-stat (1 tablet qd) or favipiravir (starting dose of 1600 mg followed by 600 mg tid) is an alternative option after the ethical review. Simultaneous use of three or more antiviral drugs is not recommended.
2、Course of Treatment
The treatment course of chloroquine phosphate should be no more than 7 days. The treatment course of other regimens has not been determined and are usually around 2 weeks. Antiviral drugs should be stopped if nucleic acid test results from sputum specimens remain negative for more than 3 times.
VII. Anti-shock and Anti-hypoxemia Treatment
During the progression from the severe to critically ill stage, patients may develop severe hypoxemia, cytokine cascade and severe infections that might develop into shock, tissue perfusion disorders, and even multiple organ failure. Treatment is aimed at incentive removal and fluid recovery. The artificial liver support system (ALSS) and blood purification can effectively diminish inflammatory mediators and cytokine cascade and prevent the incidence of shock, hypoxemia and respiratory distress syndrome.
1、Usage of Glucocorticoids when Necessary
Appropriate and short-term use of corticosteroids to inhibit cytokine cascade and to prevent disease progression should be considered for patients with severe COVID-19 pneumonia as early as possible. However, a high dose of glucocorticoids should be avoided due to adverse events and complications
1.1 Indication for Corticosteroids
① for those in severe and critically ill stage;
② for those with persistent high fever (temperature above 39°C);
③ for those whose computerized tomography (CT) demonstrated patchy ground-glass attenuation or more than 30% area of the lungs are involved;
④ for those whose CT demonstrated rapid progression (more than 50% area involved in pulmonary CT images within 48 hours);
⑤ for those whose IL-6 is above ≥ 5 ULN.
1.2 Application of Corticosteroids
Initial routine methylprednisolone at a dose of 0.75~1.5 mg/kg intravenously once a day (nearly 40 mg once or twice a day) is recommended. However, methylprednisolone at a dose of 40 mg q12h can be considered for patients with falling body temperature or for patients with significantly increased cytokines under routine doses of steroid. Even methylprednisolone at a dose of 40 mg-80 mg q12h can be considered for critical cases. Closely monitor body temperature, blood oxygen saturation, blood routine, C-reactive protein, cytokines, biochemical profile and lung CT every 2 to 3 days during the treatment as necessary. The dosage of methylprednisolone should be halved every 3 to 5 days if medical conditions of patients are improved, the body temperature normaliz-es, or involved lesions on CT are significantly absorbed. Oral methylprednisolone (Medrol) once a day is recommended when the intravenous dose is reduced to 20 mg per day. The course of corticosteroids in not defined; some experts have suggesting ceasing corticosteroids treatment when patients are nearly recovered.
1.3 Special Consideration during Treatment
① screening of TB by T-SPOT assay, HBV and HCV by antibody assay should be performed before corticosteroid therapy.
② proton pump inhibitors could be considered to prevent complications;
③ blood glucose should be monitored. High blood glucose should be treated with insulin when necessary;
④ low serum potassium should be corrected;
⑤ liver function should be monitored closely;
⑥ traditional Chinese herbal medicine may be considered for patients who are sweat-ing;
⑦ sedative-hypnotics can be administered temporarily for patients with sleep disorder.
2、Artificial Liver Treatment for Suppression of Cytokine Cascade
The artificial liver support system (ALSS) can conduct plasma exchange, adsorption, perfusion, and filtration of inflammatory mediators such as endotoxins and harmful metabolic substances of small or medium molecular weight. It can also provide serum albumin, coagulation factors, balance fluid volume, electrolytes and acid-base ratio, and manifest anti-cytokine storms, shock, lung inflammation, et al. In doing so it can also help to improve multiple organ functions including the liver and kidney. Thus, it can increase treatment success and reduce the mortality of severe patients.
2.1 Indication for ALSS
① serum inflammatory indicator (such as IL-6) level rises to ≥ 5 ULN, or rising rate is ≥1 time per day;
② involved area of pulmonary CT or X-ray images ≥10% progression per day;
③ artificial liver support system is required for the treatment of underlying diseases.Patients meeting ① + ②, or patients meeting ③.
2.2 Contraindications
There is no absolute contraindication in the treatment of critically ill patients. However, ALSS should be avoided in the following situations:
①Severe bleeding disease or disseminated intravascular coagulation;
②Those who are highly allergic to blood components or drugs used in the treatment process such as plasma, heparin and protamine;
③Acute cerebrovascular diseases or severe head injury;
④Chronic cardiac failure, cardiac functional classification ≥ grade III;
⑤Uncontrolled hypotension and shock;
⑥Severe arrhythmia.
Plasma exchange combined with plasma adsorption or dual plasma molecular adsorption, perfusion, and filtration is recommended according to the patients’ situation. 2000 mL of plasma should be exchanged when ALSS is performed. Detailed operating procedures can be found in the Expert Consensus on the Application of Artificial Liver Blood Purification System in the Treatment of Severe and Critical Novel Coronavirus Pneumonia.
ALSS significantly reduces the time that critically ill patients stay in the ICU in our hospital. Typically, the levels of serum cytokines such as IL-2/IL-4/IL-6/TNF-α are remarkably decreased, and oxygen saturation is significantly improved after ALSS.
3、Oxygen Therapy for Hypoxemia
Hypoxemia can present due to impaired respiratory functions by COVID-19. Oxygen supplementation treatment can correct hypoxemia, relieving secondary organ damage caused by respiratory distress and hypoxemia.
3.1 Oxygen therapy
(1) Continual oxygen saturation monitoring during oxygen therapy
Some patients do not necessarily have impaired oxygenation functions at the onset of infection but may manifest rapid deterioration in oxygenation over time. Therefore, continual monitoring of oxygen saturation is recommended, before and during oxygen therapy.
(2) Oxygen therapy as soon as possible
Oxygen therapy is not necessary for patients with oxygen saturation (SpO2) of more than 93% or for patients without obvious symptoms of respiratory distress without oxygen treatment. Oxygen therapy is strongly recommended to the patients with symptoms of respiratory distress. It should be noted that some severe patients with PaO2/FiO2 < 300 had no obvious symptoms of respiratory distress.
(3) Treatment goal of oxygen therapy
(4) Control oxygen therapy
PaO2/FiO2 is a sensitive and accurate indicator of oxygenation function. The stability and monitorability of FiO2 are very important for patients with disease progression and PaO2/FiO2below 300 mmHg. Controlled oxygen therapy is the preferred treatment.
High-flow nasal cannula (HFNC) oxygen therapy is recommended for patients with the following conditions: SpO2 < 93%; PaO2/FiO2 < 300 mmHg (1 mmHg # 0.133 kPa); respiratory rate > 25 times per min at bed; or remarkable progression on X-ray imaging. Patients should wear a surgical mask during HFNC treatment. The airflow of HFNC oxygen therapy should start at a low level and gradually increased up to 40-60 L/min when PaO2/FiO2 is between 200-300 mmHg so that patients do not feel obvious chest tightness and shortness of breath. An initial flow of at least 60 L/min should be given immediately for patients with obvious respiratory distress.
Tracheal intubation for patients is dependent on disease progression, systemic status and complication of patients for those with stable situation but with a low oxygenation index (<100 mmHg). Thus, detailed evaluations of the clinical condition of patients is very important before decision making. Tracheal intubation should be performed as early as possible for patients with an oxygenation index less than 150 mmHg, worsening symptoms of respiratory distress or multiple organ dysfunction within 1-2 hours after high-flow (60 L/min) and high-concentration (> 60%) HFNC oxygen therapy.
Older patients (> 60 years old) with more complications or PaO2 /FiO2 less than 200 mmHg should be treated in ICU.
3.2 Mechanical Ventilation
(1) Noninvasive Ventilation (NIV)
NIV is not strongly recommended in COVID-19 patients who fail HFNC treatment. Some severe patients progress to ARDS rapidly. Excessive inflation pressure may cause gastric distension and intolerance which contribute to aspiration and worsen lung injury. A short-term (less than 2 hours) use of NIV can be closely monitored if the patient has acute left heart failure, chronic obstructive pulmonary disease or is immunocompromised. Intubation should be performed as early as possible if improvement of respiratory distress symptoms or PaO2/FiO2 is not observed.
NIV with a double circuit is recommended. A virus filter should be installed between the mask and the exhalation valve when applying NIV with a single tube. Suitable masks should be chosen to reduce the risk of virus spread through air leakage.
(2) Invasive Mechanical Ventilation
① Principles of invasive mechanical ventilation in critically ill patients.
It is important to balance the ventilation and oxygenation demands and the risk of mechanical ventilation-related lung injury in the treatment of COVID-19 .
· Strictly set the tidal volume to 4 – 8 mL/kg. In general, the lower the lung compliance, the smaller the preset tidal volume should be.
· Maintain the platform pressure < 30 cmH2O (1 cmH2O # 0.098 kPa) and driving pressure <15 cmH2O.
· Set PEEP according to the ARDS’s protocol.
· Ventilation frequency: 18-25 times per minute. Moderate hypercapnia is allowed.
· Administer sedation, analgesia, or muscle relaxant if the tidal volume, platform pressure and driving pressure are too high.
② Lung Recruitment
Lung recruitment improves the heterogeneous distribution of lesions in patients with ARDS. However, it may result in severe respiratory and circulatory complications and therefore, the lung recruitment maneuver is not routinely recommended. The assessment of lung expandability should be performed prior to the application.
(3)Prone Position Ventilation
Most critically ill patients with COVID-19 respond well to prone ventilation, with a rapid improvement of oxygenation and lung mechanics. Prone ventilation is recommended as a routine strategy for patients with PaO2/FiO2 < 150 mmHg or with obvious imaging manifestations without contraindications. Time course recommended for prone ventilation is more than 16 hours each time. The prone ventilation can be ceased once PaO2/FiO2 is greater than 150 mmHg for more than 4 hours in the supine position.
Prone ventilation while awake may be attempted for patients who have not been intubated or have no obvious respiratory distress but with impaired oxygenation or have consolidation in gravity-dependent lung zones on lung images. Procedures for at least 4 hours each time is recommended. Prone position can be considered several times per day depending on the effects and tolerance.
(4)Prevention of Regurgitation and Aspiration
Gastric residual volume and gastrointestinal function should be routinely evaluated. Appropriate enteral nutrition is recommended to be given as earlier as possible. Nasointestinal feeding and continuous nasogastric decompression are recommended. Enteral nutrition should be suspended and aspiration with 50 mL syringe be done before transfer. If no contraindication exists, a 30° semi-sitting position is recommended.
(5)Fluid Management
Excessive fluid burden worsens hypoxemia in COVID-19 patients. To reduce pulmonary exudation and improve oxygenation, the amount of fluid should be strictly controlled while ensuring the patient’s perfusion.
(6)Strategies to Prevent Ventilator-Associated Pneumonia (VAP)
VAP bundled strategies should be strictly implemented:
① Select appropriate type of endotracheal tube;
② Use a endotracheal tube with subglottic suction (once every 2 hours, aspirated with 20 mL empty syringe each time);
③ Place the endotracheal tube at the right position and correct depth, fix properly and avoid pulling;
④ Maintain the airbag pressure at 30 – 35 cmH2O (1 cmH2O = 0.098 kPa) and monitor every 4 hours;
⑤ Monitor the airbag pressure and deal with water condensates when the position changes (two people cooperate in dumping and pouring the water condensates into a capped container containing a pre-made disinfectant chlorine solution); deal with secretions accumulated in the airbag;
⑥ Clean up secretions from the mouth and nose timely.
(7) Weaning of Ventilation
Sedatives is reduced and discontinued before awakening when the patient’s PaO2/FiO2 is more than 150 mmHg. Intubation withdrawal should be performed as earlier as possible if permitted. HFNC or NIV is used for sequential respiratory support after withdrawal.

VIII. The Rational Use of Antibiotics to Prevent Secondary Infection
COVID-19 is a disease of viral infection, therefore antibiotics are not recommended to prevent bacterial infection in mild or ordinary patients; it should be used carefully in severe patients based on their conditions. Antibiotics can be used with discretion in patients who have the following conditions: extensive lung lesions; excess bronchial secretions; chronic airway diseases with a history of pathogen colonization in the lower respiratory tract; taking glucocorticoids with a dosage ≥ 20 mg × 7d (in terms of prednisone). The options of antibiotics
include quinolones, the second or third generation cephalothins, β-lactamase inhibitor compounds, etc. The antibiotics should be used for the prevention of bacterial infection in critically severe patients, especially those with invasive mechanical ventilation. The antibiot-ics such as carbapenems, β-lactamase inhibitor compounds, linezolid and vancomycin can be used in critically ill patients according to the individual risk factors.
The patient’s symptoms, signs and indicators such as blood routine, C-reactive protein, and procalcitonin, need to be closely monitored during the treatment. When the change of a patient’s condition is detected, a comprehensive clinical judgment needs to be made. When the secondary infection cannot be ruled out, qualified specimen need to be collected for testing by smear preparation, cultivation, nucleic acid, antigen and antibody, in order to determine the infectious agent as early as possible. Antibiotics can be empirically used in the following conditions: ① more expectoration, darker sputum color, especially yellow pus sputum; ② the rise of body temperature which is not due to exacerbation of the original disease; ③ the marked increase of white blood cells and/or neutrophils; ④ procalcitonin ≥ 0.5 ng/mL; ⑤ Exacerbation of oxygenation index or circulatory disturbance that are not caused by the viral infection; and the other conditions suspiciously caused by bacteria infections.
Some COVID-19 patients are at the risk of secondary fungal infections due to weakened cellular immunity caused by viral infections, the use of glucocorticoid and/or broad-spectrum antibiotics. It is necessary to do respiratory secretions microbiological detections such as smear preparation and cultivation for critically ill patients; and provide timely D-Glucose (G-test) and galactomannan (GM-test) of blood or bronchoalveolar lavage fluid for suspected patients.
It is necessary to be vigilant with possible invasive candidiasis infection and anti-fungal therapy. Fluconazole or echinocandin can be used in the following conditions: ① patients are given broad-spectrum antibiotics for seven days or more; ② patients have parenteral nutrition; ③ patients have invasive examination or treatment; ④ patients have positive candida culture in the specimen obtained from two body parts or more; ⑤ patients have significantly increased results of G-test.
It is necessary to be vigilant with possible invasive pulmonary aspergillosis. Anti-fungal therapy such as voriconazole, posaconazole, or echinocandin are considered to be used in the following conditions: ① patients are given glucocorticoid for seven days or more; ② patients have agranulocytosis; ③ patients have chronic obstructive pulmonary disease and aspergillus culture are tested positive in the specimen obtained from the airway; ④ patients have significantly increased results of GM-test.30Handbook of COVID-19 Prevention and Treatment.
IX. The Balance of Intestinal Microecology and Nutritional Support
Some COVID-19 patients have gastrointestinal symptoms (such as abdominal pain and diarrhea) due to direct viral infection of the intestinal mucosa or antiviral and anti-infective drugs. There has been report that the intestinal microecological balance is broken in COVID-19 patients, manifesting a significant reduction of the intestinal probiotics such as lactobacillus and bifidobacterium. Intestinal microecological imbalance may lead to bacteri-al translocation and secondary infection, so it is important to maintain the balance of intesti-nal microecology by microecological modulator and nutritional support.
1、Microecologics Intervention
(1) Microecologics can reduce bacterial translocation and secondary infection. It can increase dominant gut bacteria, inhibit intestinal harmful bacteria, reduce toxin production and reduce infection caused by gut microflora dysbiosis.
(2) Microecologics can improve the gastrointestinal symptoms of patients. It can reduce water in feces, improve fecal character and defecation frequency, and reduce diarrhea by inhibiting intestinal mucosal atrophy.
(3) The hospital with relevant resources can perform intestinal flora analysis. Therefore, the intestinal flora disturbance can be discovered early according to the results. Antibi-otics can be adjusted timely and probiotics can be prescribed. These can reduce the chances of intestinal bacterial translocation and gut-derived infection.
(4) Nutrition support is an important means to maintain intestinal microecological balance.Intestinal nutrition support should be applied timely on the basis of effective evaluations of nutritional risks, gastroenteric functions, and aspiration risks.
2、Nutrition Support
The severe and critically ill COVID-19 patients who are in a state of severe stress are at high nutritional risks. Early evaluations of nutrition risk, gastrointestinal functions and aspiration risks, and timely enteral nutritional support are important to the patient’s prognosis.
(1) Oral feeding is preferred. The early intestinal nutrition can provide nutritional support, nourish intestines, improve intestinal mucosal barrier and intestinal immunity, and maintain intestinal microecology.
(2) Enteral nutrition pathway. Severe and critically ill patients often harbor acute gastrointestinal damages, manifested as abdominal distension, diarrhea, and gastroparesis. For patients with tracheal intubation, intestinal nutrition tube indwelling is recommended for post-pyloric feeding.
(3) Selection of nutrient solution. For patients with intestinal damage, predigested short peptide preparations, which are easy for intestinal absorption and utilization, are recommended. For patients with good intestinal functions, whole-protein preparations with relatively high calories can be selected. For hyperglycemia patients, nutritional preparations which are beneficial to glycemic controlling are recommended.
(4) Energy supply. 25-30 kcal per kg body weight, the target protein content is 1.2-2.0 g/kg daily.
(5) Means of nutritional supply. Pump infusion of nutrients can be used at a uniform speed, starting with a low dosage and gradually increasing. When possible, the nutrients can be heated before feeding to reduce intolerance.
(6) The elderly patients who are at high aspiration risks or patients with apparent abdominal distention can be supported by parenteral nutrition temporarily. It can be gradually replaced by independent diet or enteral nutrition after their condition improves.
X. ECMO Support for COVID-19 Patients
COVID-19 is a novel, highly infectious disease primarily targeting pulmonary alveoli, which damages primarily the lungs of critically ill patients and leads to severe respiratory failure. For the application of extracorporeal membrane oxygenation (ECMO) in COVID-19 treatment, medical professionals need to pay close attention to the following: the time and means of intervention, anticoagulant and bleeding, coordination with mechanical ventilation, awake ECMO and the early rehabilitation training, strategy of handling for complications.
1、ECMO Intervention Timing
1.1 Salvage ECMO
In the state of mechanical ventilation support, measures such as lung protective ventilation strategy and prone position ventilation have been taken for 72 h. With the onset of one of the following conditions, salvage ECMO intervention needs to be consid-ered.
(1) PaO2/FiO2 < 80 mmHg (regardless of what the PEEP level is); (2) Pplat ≤ 30 mmHg, PaCO2 > 55 mmHg;
(3) The onset of pneumothorax, air leakage > 1/3 tidal volume, duration > 48 h;
(4) Circulation deterioration, the dosage of norepinephrine > 1 μg/(kg×min);
(5) Cardio-pulmonary resuscitation in vitro life support ECPR.
1.2 Replacement ECMO
When the patient is not suitable for long-term mechanical ventilation support, i.e., the patient is not able to obtain the expected results, ECMO replacement needs to be adopt-ed immediately. With the onset of one of the following conditions, ECMO replacement needs to be considered.
(1) Decreased lung compliance. After the pulmonary recruitment maneuver, the compli-ance of the respiratory system < 10 mL/cmH2O;
(2) Persistent exacerbation of pneumomediastinum or subcutaneous emphysema. And the parameters of mechanical ventilation support cannot be reduced within 48 h, according to the estimation;
(3) PaO2/FiO2 < 100 mmHg. And it cannot be improved by routine methods in 72 h.
1.3 Early Awake ECMO
Early awake ECMO can be applied to patients who have been supported by mechanical ventilation with the expected high parameters for more than 7 days and who meet the necessary conditions of awake ECMO. They might benefit from it. All the following conditions must be met:
(1) The patient is in a clear state of consciousness and is fully compliant. He or she understands how ECMO works and its maintenance requirements;
(2) The patient is not complicated with neuromuscular diseases;
(3) Pulmonary damage score Murry > 2.5;
(4) Few pulmonary secretions. The time interval between the two airway suction procedures > 4 h;
(5) Stable hemodynamics. Vasoactive agents are not required for assistance.32Handbook of COVID-19 Prevention and Treatment
2、Cathetering Methods
Because the ECMO supporting time for most COVID-19 patients is greater than 7 days, the seldinger method should be used as much as possible for the ultrasound guided peripheral catheter insertion, which reduces the bleeding damages and infection risks brought about by intravascular cathterization by venous angiotomy, especially for the early awake ECMO patients. Intravascular catheterization by venous angiotomy may be considered only for the patients with bad blood vessel conditions, or the patients whose catheterization cannot be identified and selected by ultrasound, or the patients whose seldinger technique failed.
3、Mode Selection
(1) The first choice for the patients of respiratory impairment is the V-V mode. The V-A mode should not be the first option just because of the possible circulation problems.
(2) For the respiratory failure patients complicated with cardiac impairment, PaO2/FiO2 < 100 mmHg, the V-A-V mode ought to be selected with the total flux > 6 L/min and V/A = 0.5/0.5 is maintained by current limiting.
(3) For the COVID-19 patients without severe respiratory failure but complicated with serious cardiovascular outcomes leading to cardiogenic shock, the V-A assisted by ECMO mode ought to be selected. But IPPV support is still needed and the awake ECMO should be avoided.the awake ECMO should be avoided.
4、Flux Set-value and Target Oxygen Supply
(1) The initial flux > 80% cardiac output (CO) with a self-cycling ratio < 30%.
(2) SPO2 > 90% is to be maintained. FiO2 < 0.5 is supported by mechanical ventilation or the other oxygen therapy.
(3) To ensure the target flux, 22 Fr (24 Fr) vein access canula is the first choice for the patient with a body weight below (above) 80 kg.
5、Ventilation Setting
Normal ventilation maintenance by adjusting the sweep gas level:
(1) The initial air flow is set to be Flow: sweep gas = 1:1. The basic target is to maintain PaCO2 < 45mmHg. For the patients complicated with COPD, PaCO2 < 80% basal level.
(2) The patient’s spontaneous respiratory strength and respiratory rate (RR) should be maintained, with 10 < RR < 20 and without chief complaint of breathing difficulty from the patient.
(3) The sweep gas setup of the V-A mode needs to ensure the 7.35-7.45 PH value of the bloodstream out of the oxygenator membrane.
6、Anti-Coagulation and Bleeding Prevention
(1) For the patients without active bleeding, without visceral bleeding, and with platelet count > 50×109/L, the recommended initial heparin dosage is 50 U/kg.
(2) For the patients complicated with bleeding or with platelet count < 50×109/L, the recommended initial heparin dosage is 25 U/kg.
(3) The activated partial thromboplastin time (aPPT) being 40—60 sec is proposed to be the target of anticoagulation maintenance dosage. The trend of D-dimer change should be considered at the same time.345633Handbook of COVID-19 Prevention and Treatment.
(4) Heparin-free operation may be performed in the following circumstances: the ECMO support must continue but there is fatal bleeding or active bleeding that has to be controlled; whole heparin coated loop and catheterization with blood flow > 3 L/min. The recommend operation time < 24 hour. Replacement devices and consumables need to be prepared.
(5) Heparin resistance. Under some conditions of heparin usage, aPTT is not able to reach the standard and blood coagulation happens. In this case, the activity of plasma antithrombin III (ATIII) needs to be monitored. If the activity reduces, fresh frozen plasma needs to be supplemented to restore heparin sensitivity.
(6) Heparin induced thrombopenia (HIT). When HIT happens, we recommend to perform plasma exchange therapy, or to replace heparin with argatroban.
7、Weaning from ECMO and Mechanical Ventilation
(1) If a patient treated by V-V ECMO combined with mechanical ventilation satisfies the awake ECMO condition, we suggest to first try to remove the artificial airway, unless the patient has ECMO related complications, or the expected time of removal of all the assisting machines is less than 48 h.
(2)For a patient who has too much airway secretions that frequent artificial suction clearance is needed, who is expected to have a long-term mechanical ventilation support, who satisfies the conditions PaO2/FiO2 > 150 mmHg and time > 48 h, whose lung image changes for the better, and whose damages related to mechanical ventilation pressure have been controlled, the ECMO assistance may be removed. It is not recom-mended to keep ECMO intubation.


XI. Convalescent Plasma Therapy for COVID-19 Patients
Since Behring and Kitasato reported the therapeutic effects of diphtheria antitoxin plasma in 1891, plasma therapy has become an important means of pathogen immunotherapy for acute infectious diseases. The disease progression is rapid for severe and critically ill patients of an emerging infectious disease. In the early phase, the pathogens damage the target organs directly and then lead to severe immuno-pathological damage. The passive immune antibodies can effectively and directly neutralize the pathogens, which reduces the damage of the target organs and then block the subsequent immune-pathological damages. During multiple global pandemic outbreaks, WHO also emphasized that “convalescent plasma the rapy is one of the most recommended potential therapies, and it has been used during other epidemic outbreaks”. Since the outbreak of COVID-19, the initial mortality rate was rather high due to the lack of specific and effective treatments. As mortality rate is an important metric that the public concerns, clinic treatments which can reduce the fatality rate of critical cases effectively are key to avoid public panic. As a provincial-level hospital in Zhejiang province, we have been responsible to treat the patients from Hangzhou and the critically ill patients of the province. There are abundant potential convalescent plasma donors and critically ill patients who need convalescent plasma treatment in our hospital.
1、Plasma collectionIn
addition to the common requirements of blood donation and procedures, the following details should be noted.
1.1 Donors
At least two weeks after recovery and being discharged (the nucleic acid test of the sample taken from the lower respiratory tract remains negative≥14 days). 18 ≤ Age ≤ 55. The body weight>50 kg (for male) or >45 kg (for female). At least one week since last glucocorticoid usage. More than two weeks since last blood donation.
1.2 Collection Method Plasmapheresis, 200-400 mL each time (based on medical consultation).
1.3 Post-Collection Testing In addition to the general quality test and the test of blood-borne disease, the blood samples need to be tested for:
(1) Nucleic acid testing for SARS-CoV-2;
(2) 160-fold dilution for the qualitative test of SARS-CoV-2 specific IgG and IgM detection; or 320-fold dilution for the qualitative test of whole antibody detection. If possible, keep > 3 mL plasma for the viral neutralization experiments.
The following should be noted. During the comparison of virus neutralization titer and luminescent IgG antibody quantitative detection, we found that the present SARS-CoV-2 specific IgG antibody detection does not fully demonstrate the actual virus neutralization capability of the plasma. Therefore, we suggested the virus neutralization test as the first choice, or test the overall antibody level with the 320-fold dilution of the plasma
2、Clinical Use of the Convalescent Plasma
2.1 Indication
(1) Severe or critically ill COVID-19 patients tested positive in respiratory tract test;
(2) The COVID-19 patients who are not severe or critically ill, but in a state of immunity suppression; or have low CT values in the virus nucleic acid testing but with a rapid disease progression in the lungs.
Note: In principle, the convalescent plasma should not be used on COVID-19 patients with disease course exceeding three weeks. But in clinical applications, we found that the convalescent plasma therapy is effective for patients with a disease course exceeding three weeks and whose virus nucleic acid tests continuously to show positive from respiratory tracts specimen. It can speed up virus clearance, increase the numbers of the plasma lymphocytes and NK cells, reduce the level of plasma lactic acid, and improve renal functions.
2.2 Contraindication
(1)Allergy history of plasma, sodium citrate and methylene blue;
(2) For patients with history of autoimmune system diseases or selective IgA deficiency, the application of convalescent plasma should be evaluated cautiously by clinicians.
2.3 Infusion plan In general, the dosage of convalescent plasma therapy is ≥400 mL for one infusion, or ≥ 200 mL per infusion for multiple infusions.
XII. TCM Classification Therapy to Improve Curative Efficacy
1、Classification and Stage
COVID-19 can be divided into early, middle, critical and recovery stages. At the early stage, the disease has two main types: “wet lungs” and “external cold and internal heat.” The middle stage is characterized by “intermittent cold and heat.” The critical stage is characterized by “internal block of epidemic toxin.” The recovery stage is characterized by “qi deficiency in lung-spleen.” The disease initially belongs to wet lung syndrome. Due to fever, both intermittent cold and heat treatments are recom-mended. In the middle stage, cold, dampness, and heat coexist, belonging to “cold-heat mixture” in terms of TCM. Both cold and heat therapy should be consid-ered. According to the theory of TCM, heat should be treated with cold drugs. But cold drugs impair Yang and lead to a cold spleen and stomach and cold-heat mixture in the middle-Jiao. Therefore, in this stage both cold and heat therapies should be consid-ered. Because cold-heat symptoms are commonly seen in COVID-19 patients, the cold-heat therapy is better than other approaches.
2、Therapy Based on Classification
(1) Wet lungs Ephedra Herb 6 g, Semen Armeniacae Amarumg 10 g, Coix Seed 30 g, Liquoric Root 6 g, Baical Skullcap Root 15 g, Huoxiang 10 g, Reed Rhizome 30 g, Cyrtomi-um Rhizome 15 g, Indian Buead 20 g, Chinese Atractylodes Rhizome 12 g, Officinal Magnolia Bark 12 g.
(2) External cold and internal heatHerba Ephedrae 9 g, Raw Gypsum Fibrosum 30 g, Semen Armeniacae Amarumg 10 g, Liquoric Root 6 g, Baical Skullcap Root 15 g, Pericarpium Trichosanthis 20 g, Fructus Aurantii 15 g, Officinal Magnolia Bark 12 g, Tripterospermum Cordifolium 20 g, White Mulberry Root-bark 15 g, Pinellia Tuber 12 g, Indian Buead 20 g, Platycodon Root 9 g.
(3) Intermittent cold-heatPinellia Tuber 12 g, Baical Skullcap Root 15 g, Golden Thread 6 g, Dried Ginger 6 g, Chinese Date 15 g, Kudzuvine Root 30 g, Costustoot 10 g, Indian Buead 20 g, Thunberg Fritillary Bulb 15 g, Coix Seed 30 g, Liquoric Root 6 g.
(4) Internal block of epidemic toxinUse cheongsimhwan for treatment.
(5) Qi deficiency of lung and spleen
Membranous Milkvetch Root 30 g, Pilose Asiabell Root 20 g, Roasted Largehead Atractylodes Rhizome 15 g, Indian Buead 20 g, Fructus Amomi 6 g, Siberian Solomon-seal Rhizome 15 g, Pinellia Tuber 10 g, Tangerine Peel 6 g, Wingde Yan Rhizome 20 g, Semen Nelumbinis 15 g, Chinese Date 15 g.
Patients in different stages should take different approaches. One dose per day. Boil the medicine in water. Take it every morning and evening.
XIII. Drug Use Management of COVID-19 Patients
COVID-19 patients are often complicated with underlying diseases receiving multiple types of drugs. Therefore, we should pay more attention to the adverse drug reactions and drug interactions so as to avoid drug-induced organ damage and improve the success rate of treatment.
1、Identification of adverse drug reactions
It has been demonstrated that the incidence of abnormal liver function is 51.9% in COVID-19 patients who have received lopinavir/ritonavir combined arbidol antiviral treatment. Multivariate analysis revealed that antiviral agents and more concomitant medications are two independent risk factors of abnormal liver function. Therefore, monitoring of the adverse drug reactions should be strengthened; the unnecessary drug combinations should be reduced. The main adverse reactions of antiviral agents include:
(1) Lopinavir /ritonavir and darunavir/cobicistat: diarrhea, nausea, vomit, the increase of serum aminotransferase, jaundice, dyslipidemia, the increase of lactic acid. Symptoms will recover after drug withdrawal.
(2) Arbidol:the increase of serum aminotransferase and jaundice. When combined with lopinavir, the incidence rate is even higher. The symptoms will recover after drug withdrawal. Sometimes a slowdown of the heart could be induced; thus it is necessary to avoid the combination of arbidol with β–receptor inhibitors such as metoprolol and propranolol. We suggest to stop taking the drugs when the heart rate drops below 60/min.
(3) Fapilavir: elevation of plasma uric acid, diarrhea, neutropenia, shock, fulminant hepatitis, acute kidney injury. The adverse reactions were commonly seen in elderly patients or patients complicated with cytokine storm.
(4) Chloroquine phosphate: dizziness, headache, nausea, vomit, diarrhea, different kinds of skin rash. The most severe adverse reaction is cardiac arrest. The main adverse reaction is the ocular toxicity. An electrocardiogram needs to be examined before taking the drug. The drug should be prohibited for patients with arrhythmia (e.g., conduction block), retinal disease, or hearing loss.
2、Therapeutic Drug Monitoring
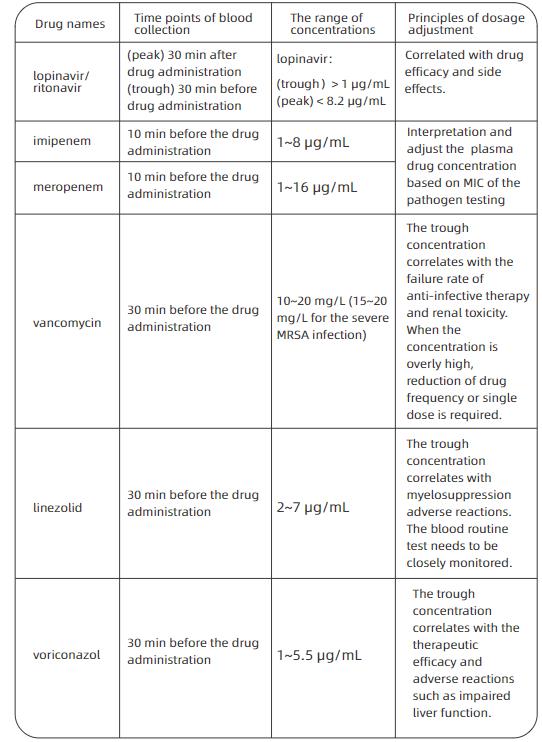
Some antiviral and antibacterial drugs need therapeutic drug monitoring (TDM). Table 1 presents the plasma concentrations of such drugs and their dosage adjustment. Upon the onset of aberrations of plasma drug concentration, the treatment regimens need to be adjusted by considering the clinical symptoms and concomitant drugs
Table 1 The range of concentrations and points for attention of the common TDM drugs for the COVID-19 patients
3、Paying attention to the potential drug interactions
Antiviral drugs such as lopinavir/ritonavir are metabolized through the enzyme CYP3A in the liver. When patients receiving concomitant medications, the potential drug interactions need to be carefully screened. Table 2 shows interactions between antiviral drugs and common drugs for underlying diseases.
Table 2 Interactions between antiviral drugs and common drugs for underlying
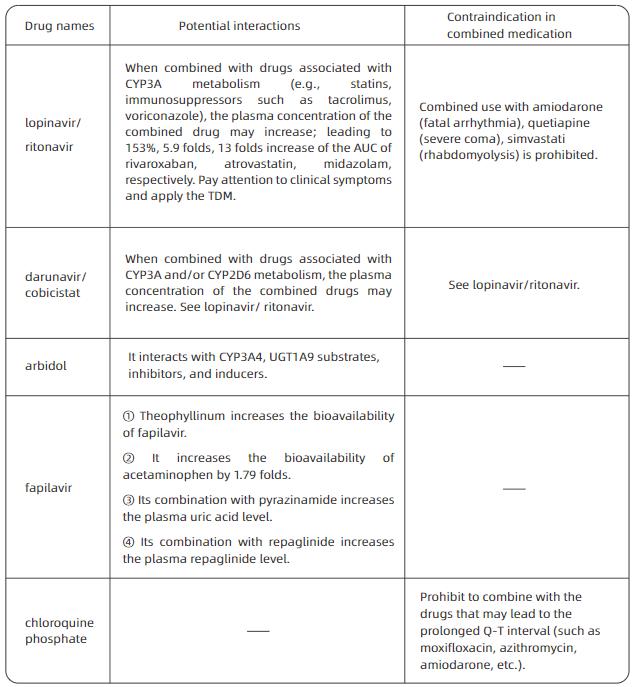
Note:“—”: no relevant data;TDM:therapeutic drug monitoring;AUC:area under the curve;UGT1A9:uridine diphosphate glucosidase 1A9.
4、Avoiding medical damage in special populations
Special populations include pregnant women, patients with hepatic and renal insufficien-cy, patients supported by mechanical ventilation, patients under continuous renal replacement therapy (CRRT) or, extracorporeal membrane oxygenation (ECMO), etc. The following aspects need to be noted during drug administration.

XIV. Psychological Intervention with COVID-19 Patients
1、The psychological stress and symptoms of COVID-19 patients
Confirmed COVID-19 patients often have symptoms such as regret and resentment, loneliness and helplessness, depression, anxiety and phobia, irritation and sleep deprivation. Some patients may have panic attacks. Psychological evaluations in the isolated wards demonstrated that, about 48% of confirmed COVID-19 patients manifested psychological stress during early admission, most of which were from their emotional response to stress. The percentage of delirium is high among the critically ill patients. There is even a report of encephalitis induced by the SARS-CoV-2 leading to psychological symptoms such as unconsciousness and irritability.
2、Establishing a dynamic mechanism for evaluation and warning of psycholog-ical crisis
Patients’ mental states (individual psychological stress, mood, sleep quality, and pressure) should be monitored every week after admission and before discharge. The self-rating tools include: Self-Reporting Questionnaire 20 (SRQ-20), Patient Health Questionnaire 9 (PHQ-9) and Generalized Anxiety Disorder 7 (GAD-7). The peer-rating tools include: Hamilton Depression Rating Scale (HAMD), Hamilton Anxiety Rating Scale (HAMA), Positive and Negative Syndrome Scale (PANSS). In such a special environment as the isolated wards, we suggest that patients should be guided to complete the questionnaires through their cell phones. The doctors can interview and perform scale assessing through face-to-face or online discussion.
3、Intervention and treatment based on the assessment
3.1 Principles of intervention and treatment
For mild patients, psychological intervention is suggested. Psychological self-adjust-ment includes breathing relaxation training and mindfulness training. For moderate to severe patients, intervention and treatment by combining medication and psychother-apy are suggested. New antidepressants, anxiolytics, and benzodiazepines can be prescribed to improve the patients’ mood and sleep quality. The second generation antipsychotics such as olanzapine and quetiapine can be used to improve psychotic symptoms such as illusion and delusion.
3.2 The recommendation of psychotropic medications in elderly patients
Middle-aged or elderly COVID-19 patients’ medical situations are often complicated by physical diseases such as hypertension and diabetes. Therefore, when selecting psychotropic medications, the drug interactions and their effects on respiration must be fully considered. We recommend using citalopram, escitalopram, etc. to improve depression and anxiety symptoms; benzodiazepines such as estazolam, alprazolam, etc. to improve anxiety and sleep quality; olanzapine, quetiapine, etc. to improve psychotic symptoms.
XV. Rehabilitation Therapy for COVID-19 Patients
Severe and critically ill patients suffer from different degrees of dysfunction, especially respiratory insufficiency, dyskinesia and cognitive impairment, during both acute and recovery stages.
1、Rehabilitation therapy for severe and critically ill patients
The goal of early rehabilitation intervention is to reduce breathing difficulties, relieve symptoms, ease anxiety and depression and lower the incidence of complications. The process of early rehabilitation intervention is: rehabilitation assessment – therapy – reassessment.
1.1 Rehabilitation assessment
Based on general clinical assessment, especially functional evaluation, including respiration, cardiac status, motion and ADL should be emphasized. Focus on respiratory rehabilitation assessment, which includes the evaluation of thoracic activity, diaphragm activity amplitude, respiratory pattern and frequency, etc.
1.2 Rehabilitation therapy
The rehabilitation therapy of severe or critically ill COVID-19 patients mainly includes position management, respiratory training, and physical therapy.
(1) Position management. Postural drainage may reduce the influence of sputum on the respiratory tract, which is especially important to improve the patient’s V/Q. Patients must learn to tip themselves into a position which allows gravity to assist in draining excretion from lung lobes or lung segments. For patients using sedatives and suffering from consciousness disturbance, a standing-up bed or the bed head elevation (30°-45°-60°) may be applied if the patient’s condition permits. Standing is the best body position for breathing in a resting state, which can effectively increase the patient’s respiratory efficiency and maintain lung volume. As long as the patient feels good, let the patient take a standing position and gradually increase the time standing.
(2) Respiratory exercise. Exercise can fully expand the lungs, help the excretions from pulmonary alveoli and airway expel into the large airway so that sputum would not accumulate at the bottom of the lungs. It increases the vital capacity and enhances lung function. Deep-slow breathing and chest expansion breathing combined with shoulder expansion are the two major techniques of respiratory exercises.
① Deep-slow breathing: while inhaling, the patient should try his/her best to move the diaphragm actively. The breathing should be as deep and slow as possible to avoid the reduction of respiratory efficiency caused by fast-shallow breathing. Compared with thoracic breathing, this kind of breathing needs less muscle strength but has better tidal volume and V/Q value, which can be used to adjust breathing when experiencing short of breath.
② Chest expansion breathing combined with shoulder expansion: Increase pulmonary ventilation. When taking a deep-slow breath, one expands his/her chest and shoulders while inhaling; and moves back his/her chest and shoulders while exhaling. Due to the special pathological factors of viral pneumonia, suspending breathing for a long time should be avoided in order not to increase the burden of respiratory function, and the heart, as well as oxygen consumption. Meanwhile, avoid moving too fast. Adjust the respiratory rate at 12-15 times/min.43Handbook of COVID-19 Prevention and Treatment
(3) Active cycle of breathing techniques. It can effectively remove bronchus excretion and improve lung function without exacerbation of hypoxemia and airflow obstruction. It consists of three stages (breathing control, thoracic expansion and exhalation). How to form a cycle of breathing should be developed according to the patient’s condition.
(4) Positive expiratory pressure trainer. The pulmonary interstitium of COVID-19 patients has been severely damaged. In mechanical ventilation, low pressure and low tidal volume are required to avoid damages to the pulmonary interstitium. Therefore, after the removal of mechanical ventilation, positive expiratory pressure trainer can be used to help the movement of excretions from the low volume lung segments to the high-vol-ume segments, lowering the difficulty of expectoration. Expiratory positive pressure can be generated through air flow vibration, which vibrates the airway to achieve airway supporting. The excretions can then be removed as the high-speed expiratory flow moves the excretions.
(5) Physical therapy. This includes ultrashort wave, oscillators, external diaphragm pacemaker, electrical muscle stimulation, etc.
XVI. Lung Transplantation in Patients with COVID-19
Lung transplantation is an effective treatment approach for final-stage chronic lung diseases. However, it is rarely reported that lung transplantation has been performed to treating acute infectious lung diseases. Based on current clinical practice and results, FAHZU summarized this chapter as a reference for medical workers. In general, following the principles of exploration, doing the best to save life, highly selective and high protection, if lung lesions are not significantly improved after adequate and reasonable medical treatment, and the patient is in critical condition, lung transplantation could be considered with other evalua-tions.
1、Pre-transplantation assessment
(1) Age: It is recommended that the recipients are not older than 70. Patients over 70 years old are subject to careful evaluation of other organ functions and postoperative recovery capability.
(2) The course of the disease: There is no direct correlation between the length of the disease course and the severity of the disease. However, for patients with short disease courses (fewer than 4-6 weeks), a full medical assessment is recommended to evaluate whether adequate medication, ventilator assistance, and ECMO support have been provided.
(3) Lung function status: Based on the parameters collected from lung CT, ventilator, and ECMO, it is necessary to evaluate whether there is any chance of recovery.
(4) Functional assessment of other major organs: a. Evaluation of the consciousness status of patients in critical condition using brain CT scan and electroencephalography is crucial, as most of them would have been sedated for an extended period; b. Cardiac assessments, including electrocardiogram and echocardiography that focus on right heart size, pulmonary artery pressure and left heart function, are highly recommend-ed; c. The levels of serum creatinine and bilirubin should also be monitored; for patients with liver failure and renal failure, they should not be subjected to lung transplantation until the functions of the liver and kidney are recovered.
(5) The nucleic acid test of COVID-19: The patient should be tested negative for at least two consecutive nucleic acid tests with a time interval longer than 24 hours. Given the increased incidents of COVID-19 test result returning from negative to positive after treatment, it is recommended to revise the standard to three consecutive negative results. Ideally, negative results should be observed in all body fluid samples, including blood, sputum, nasopharynx, broncho-alveolar lavage, urine, and feces. Considering the difficulty in operation, however, at least the testing of sputum and broncho-alveolar lavage samples should be negative.
(6) Assessment of infection status: With the extended in-patient treatment, some COVID-19 patients may have multiple bacterial infections, and thus a full medical assessment is recommended to evaluate the situation of infection control, especially for multidrug-resistant bacterial infection. Moreover, post-procedure antibacterial treatment plans should be formed to estimate the risk of post-procedure infections.
(7) The preoperative medical assessment process for lung transplantation in COVID-19 patients: a treatment plan proposed by the ICU team → multidisciplinary discussion → comprehensive medical evaluation → analysis and treatment of relative contraindica-tions → pre-habilitation before lung transplantation.144Handbook of COVID-19 Prevention and Treatment
2、Contraindications
Please refer to The 2014 ISHLT Consensus: A consensus document for the selection of lung transplantation candidates issued by the International Society for Heart and Lung Transplantation (updated in 2014).
XVII. Discharge Standards and Follow-up Plan for COVID-19 Patients
1、Discharge standards
(1) Body temperature remains normal for at least 3 days (ear temperature is lower than 37.5 °C);
(2) Respiratory symptoms are significantly improved;
(3) The nucleic acid is tested negative for respiratory tract pathogen twice consecutively (sampling interval more than 24 hours); the nucleic acid test of stool samples can be performed at the same time if possible;
(4) Lung imaging shows obvious improvement in lesions;
(5) There is no comorbidities or complications which require hospitalization;
(6) SpO2 > 93% without assisted oxygen inhalation;
(7) Discharge approved by multi-disciplinary medical team.
2、Medication after discharge
Generally, antiviral drugs are not necessary after discharge. Treatments for symptoms can be applied if patients have mild cough, poor appetite, thick tongue coating, etc. Antiviral drugs can be used after discharge for patients with multiple lung lesions in the first 3 days after their nucleic acid are tested negative.
3、Home isolation
Patients must continue two weeks of isolation after discharge. Recommended home isolation conditions are:
① Independent living area with frequent ventilation and disinfection;
② Avoid contacting with infants, the elderly and people with weak immune functions at home;
③ Patients and their family members must wear masks and wash hands frequently;
④ Body temperature are taken twice a day (in the morning and evening) and pay close attention to any changes in the patient’s condition.
4、Follow-up
A specialized doctor should be arranged for each discharged patient’s follow-ups. The first follow-up call should be made within 48 hours after discharge. The outpatient follow-up will be carried out 1 week, 2 weeks, and 1 month after discharge. Examina-tions include liver and kidney functions, blood test, nucleic acid test of sputum and stool samples, and pulmonary function test or lung CT scan should be reviewed according to the patient’s condition. Follow-up phone calls should be made 3 and 6 months after discharge.445Handbook of COVID-19 Prevention and Treatment
5、Management of patients tested positive again after discharge
Strict discharge standards have been implemented in our hospital. There is no discharged case in our hospital whose sputum and stool samples are tested positive again in our follow-ups. However, there are some reported cases that patients are tested positive again, after being discharged based on the standards of national guidelines (negative results from at least 2 consecutive throat swabs collected at an interval of 24 hours; body temperature remaining normal for 3 days, symptoms signifi-cantly improved; obvious absorption of inflammation on lung images). It is mainly due to sample collection errors and false negative testing results. For these patients, the following strategies are recommended:
(1) Isolation according to the standards for COVID-19 patients.
(2) Continuing to provide antiviral treatment which has been proved to be effective during prior hospitalization.
(3) Discharge only when improvement is observed on lung imaging and the sputum and stool are tested negative for 3 consecutive times (with an interval of 24 hours).
(4) Home isolation and follow-up visits after discharge in accordance with the require-ments mentioned above.

